Most heart attacks occur when vulnerable plaque ruptures,1 with a resulting thrombosis.2 Yet evaluation of individual vulnerable plaque to identify characteristics of the plaque itself has been less than predictive for coronary and thrombotic events.3-4 Further, plaque often ruptures without clinical symptoms or coronary events.5 When arterial health is compromised, plaque ruptures can lead to major coronary events.
To address this reality, a shift has happened, from assessing individual plaque to assessing total plaque burden. Looking at any individual plaque in the body is a slice of overall arterial health, while plaque burden provides a broader view of overall risk. Furthermore, the traditional risk factors for cardiac disease like obesity, tobacco use, high blood pressure, and Type 2 diabetes, may need to be expanded to provide truly personalized treatment.
As one group of authors stated, referring to the traditional risk factors for cardiovascular health:
“The current risk-factor assessment is innately flawed as it fails to treat people individually based on the presence of arterial inflammation and non-obstructive disease. Often patients receive treatments that are unnecessary and many cause harm.”6
One key expansion is to consider the health of the arterial walls: “it is imperative that the study of atherosclerosis focus on the wall of the artery where plaque is identified at its most vulnerable state.”5 In this context, understanding which patients are at higher risk includes assessing the health of the arterial wall as well as other factors. A combination of multiple factors may make patients more vulnerable to coronary events.
For truly preventative, precision care, taking a systems approach and working with vulnerable patients must be the core of intervention, rather than single plaque analysis.5
New emphasis: The endothelial glycocalyx
There is a fundamental structure in the blood vessels for monitoring and understanding endothelial health: the endothelial glycocalyx (or EGX). The EGX is the micro-thin, gel-like lining on the luminal surface of every blood vessel.
The EGX is a selective permeability barrier,7 as well as a mediator of inflammatory response in the blood vessels. Inflammation, endotoxins, oxidative stress and more factors can damage the EGX, causing it to become less slippery and develop gaps.8 When the EGX breaks down, plaque is more likely to develop and progress, reducing arterial elasticity and increasing the chance of thrombosis.
Maintaining blood vessel integrity in atherosclerosis
In a 2019 Journal of the American College of Cardiology review article, authors described the triangle of focus for promoting cardiovascular health in patient-centered care is as follows: “prothrombotic milieu, atheroma burden, and disease activity.”5
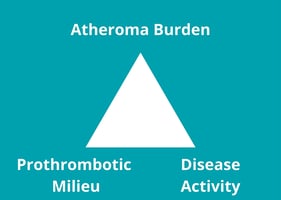 As a core element in all three of these factors, maintaining EGX integrity takes center stage.
As a core element in all three of these factors, maintaining EGX integrity takes center stage.
Atheroma burden and the EGX
Atheroma is the buildup of plaque along the inside of the artery walls. When significant, this buildup of plaque becomes atherosclerosis, which is a turning point for cardiovascular risk. As the protective, slippery barrier between the endothelium and the blood, the EGX is a single point of failure that benefits from protection.
When the EGX breaks down, atheroma increases. This relationship is so strong some authors have suggested EGX as a biomarker for atherosclerotic risk.9
In models of arterial flow, a healthy EGX shows protective power even when high blood pressure and LDL are present at the same time.10 A mouse study showed that a reduced EXG resulted in higher intimal wall plaque levels.11
Prothrombotic milieu & the EGX
The role of thrombosis in coronary events has drawn increasing interest. As one large, nested, case-control study found, stenosis and narrowing of the arteries was not present in the majority of patients with acute coronary syndrome.12 The patient’s thrombotic potential and plaque burden seem to be more important than stenosis.
Importantly, the EGX houses coagulation factors. In conditions like sepsis where the endothelium is compromised, so is blood coagulation.13 In a case series, EGX damage preceded delayed cerebral ischemia, suggesting that the EGX modulates cerebral microthrombosis.14 Hyperglycemia, which damages the EGX, is also related to poor thrombotic outcomes.15 In a mouse study, superoxide dismutase (which is present in the EGX) was protective against both arterial and venous thrombosis.16 Furthermore, in vivo studies have highlighted that the EGX may play a mediating role in thrombosis.17
Disease activity and the EGX
Taking a step back, understanding a patient’s plaque progression over time helps to contextualize the frequency of plaque rupture and possible thrombotic events. If a patient moves from having low plaque burden to high plaque burden, ruptures and scarring are more frequent. This produces a prothrombotic milieu. On the other hand, if a patient has plaque regression, thrombosis potential decreases.
Endothelial shear stress has been raised as a new factor influencing the pathogenesis of atherosclerosis as well as the formation of dangerous plaque.18 As one review article states, “the majority of ruptures occur on the upstream side of the plaques and result from low ESS and high local wall stress.”15 This is particularly interesting in the context of the EGX, since shear stress directly affects the functions of the EGX.
Decreasing overall inflammation is another possible strategy to lower disease burden. Inflammation is highly correlated with atherosclerotic disease activity.19 As the selective permeability barrier for the endothelium, the EGX is highly responsive to inflammation. For instance, in a murine cell study, experimentally-induced inflammation led to degradation of the EGX.20 In a study on patients receiving cardiac surgery, inflammation also led to damage of the EGX.21
With the advent of CIMT, tracking plaque progression in primary care has become doable. By assessing the health of the blood vessels, primary care clinicians and cardiologists alike can provide newfound predictive capabilities for patients at risk of coronary events.
Why upstream intervention?
Interventions that promote EGX health have resulted in improved patient outcomes. Although research into the EGX and cardiovascular disease in general is ongoing, support and protection of the EGX is becoming an important clinical priority.
As the current cardiology care model continues to evolve and recognize the importance of the integrity of blood vessel walls, EGX support is emerging as a powerful tool for early prevention, personalized treatment, and recovery after a cardiac event.
Learn more with this 20-minute presentation by Dr. Kristine Burke, exploring the latest science around the EGX and its clinical impacts.
References
-
Small GR, Chow BJW. CT Imaging of the Vulnerable Plaque. Curr Treat Options Cardiovasc Med. 2017;19(12):92. Published 2017 Nov 6. doi:10.1007/s11936-017-0592-9
-
Fishbein MC. The vulnerable and unstable atherosclerotic plaque. Cardiovasc Pathol. 2010;19(1):6-11. doi:10.1016/j.carpath.2008.08.004
-
Arbab-Zadeh A, Fuster V. The myth of the "vulnerable plaque": transitioning from a focus on individual lesions to atherosclerotic disease burden for coronary artery disease risk assessment. J Am Coll Cardiol. 2015;65(8):846-855. doi:10.1016/j.jacc.2014.11.041
-
Hafiane A. Vulnerable Plaque, Characteristics, Detection, and Potential Therapies. J Cardiovasc Dev Dis. 2019;6(3):26. Published 2019 Jul 27. doi:10.3390/jcdd6030026
-
Arbab-Zadeh A, Fuster V. From Detecting the Vulnerable Plaque to Managing the Vulnerable Patient: JACC State-of-the-Art Review. J Am Coll Cardiol. 2019;74(12):1582-1593. doi:10.1016/j.jacc.2019.07.062
-
Doneen AL, Bale BF, Vigerust DJ, Leimgruber PP. Cardiovascular Prevention: Migrating From a Binary to a Ternary Classification. Front Cardiovasc Med. 2020;7:92. Published 2020 May 22. doi:10.3389/fcvm.2020.00092
-
Radeva MY, Waschke J. Mind the gap: mechanisms regulating the endothelial barrier. Acta Physiol (Oxf). 2018;222(1):10.1111/apha.12860. doi:10.1111/apha.12860
-
Pillinger NL, Kam P. Endothelial glycocalyx: basic science and clinical implications. Anaesth Intensive Care. 2017;45(3):295-307. doi:10.1177/0310057X1704500305
-
Xue XJ, Jiang Y, Chen L, Chen SL. Relationship between the endothelial glycocalyx and the extent of coronary atherosclerosis. Microcirculation. 2018;25(8):e12504. doi:10.1111/micc.12504
-
Liu X, Fan Y, Deng X. Effect of the endothelial glycocalyx layer on arterial LDL transport under normal and high pressure. J Theor Biol. 2011;283(1):71-81. doi:10.1016/j.jtbi.2011.05.030
-
van den Berg BM, Spaan JA, Vink H. Impaired glycocalyx barrier properties contribute to enhanced intimal low-density lipoprotein accumulation at the carotid artery bifurcation in mice. Pflugers Arch. 2009;457(6):1199-1206. doi:10.1007/s00424-008-0590-6
-
Chang HJ, Lin FY, Lee SE, et al. Coronary Atherosclerotic Precursors of Acute Coronary Syndromes. J Am Coll Cardiol. 2018;71(22):2511-2522. doi:10.1016/j.jacc.2018.02.079
-
Schouten M, Wiersinga WJ, Levi M, van der Poll T. Inflammation, endothelium, and coagulation in sepsis. J Leukoc Biol. 2008;83(3):536-545. doi:10.1189/jlb.0607373
-
Bell JD, Rhind SG, Di Battista AP, Macdonald RL, Baker AJ. Biomarkers of Glycocalyx Injury are Associated with Delayed Cerebral Ischemia Following Aneurysmal Subarachnoid Hemorrhage: A Case Series Supporting a New Hypothesis. Neurocrit Care. 2017;26(3):339-347. doi:10.1007/s12028-016-0357-4
-
Lemkes BA, Hermanides J, Devries JH, Holleman F, Meijers JC, Hoekstra JB. Hyperglycemia: a prothrombotic factor?. J Thromb Haemost. 2010;8(8):1663-1669. doi:10.1111/j.1538-7836.2010.03910.x
-
Dayal S, Gu SX, Hutchins RD, et al. Deficiency of superoxide dismutase impairs protein C activation and enhances susceptibility to experimental thrombosis. Arterioscler Thromb Vasc Biol. 2015;35(8):1798-1804. doi:10.1161/ATVBAHA.115.305963
-
Nieuwdorp M, van Haeften TW, Gouverneur MC, et al. Loss of endothelial glycocalyx during acute hyperglycemia coincides with endothelial dysfunction and coagulation activation in vivo. Diabetes. 2006;55(2):480-486. doi:10.2337/diabetes.55.02.06.db05-1103
-
Lee KY, Chang K. Understanding Vulnerable Plaques: Current Status and Future Directions. Korean Circ J. 2019;49(12):1115-1122. doi:10.4070/kcj.2019.0211
-
Libby P, Loscalzo J, Ridker PM, et al. Inflammation, Immunity, and Infection in Atherothrombosis: JACC Review Topic of the Week. J Am Coll Cardiol. 2018;72(17):2071-2081. doi:10.1016/j.jacc.2018.08.1043
-
Lipowsky HH. Relative shedding of glycosaminoglycans from the endothelial glycocalyx during inflammation and their contribution to stiffness of the glycocalyx. Biorheology. 2019;56(2-3):191-205. doi:10.3233/BIR-190225
-
Pesonen E, Passov A, Andersson S, et al. Glycocalyx Degradation and Inflammation in Cardiac Surgery. J Cardiothorac Vasc Anesth. 2019;33(2):341-345. doi:10.1053/j.jvca.2018.04.007
IMPORTANT NOTICE:
The information on this webpage is for licensed healthcare practitioner education only, and is not to be disseminated to the general public.



