Early detection, early prevention, and arterial plaque

A recent article in JAMA highlighted an emerging challenge in the field of vascular health.1 Arterial calcification has long been known as a vascular risk marker for asymptomatic individuals. For many, plaque buildup is being detected earlier.
Recent enhancements in coronary artery calcification scoring (CAC) have enabled quantification of atherosclerosis across a far wider spectrum of severity. For clinicians focused on preventative care, this development challenges conventional assessments of risk.
At what point along the spectrum is intervention called for, and which protocol is best adapted to which risk level?
This JAMA article provided a hypothetical case of a 45-year old male which is worth quoting in detail to illustrate the challenge. In this imagined case, the following data is presented:
- CAC score: 50 Agatston units (91st percentile for age, sex, and ethnicity).
- Total serum cholesterol, 189 mg/dL
- LDL-C 122 mg/dL
- HDL-C 45 mg/dL
- Triglycerides, 109 mg/dL
- Hemoglobin A level 5.4
The individual is described as a lifelong nonsmoker with no family history of premature coronary artery disease or myocardial infarction.
Here’s where the challenge emerges. The pooled cohort equations estimate for this patient a 10-year atherosclerotic cardiovascular disease (ASCVD) event risk of 1.2%.
The danger he faces, in other words, is very low — but above zero.
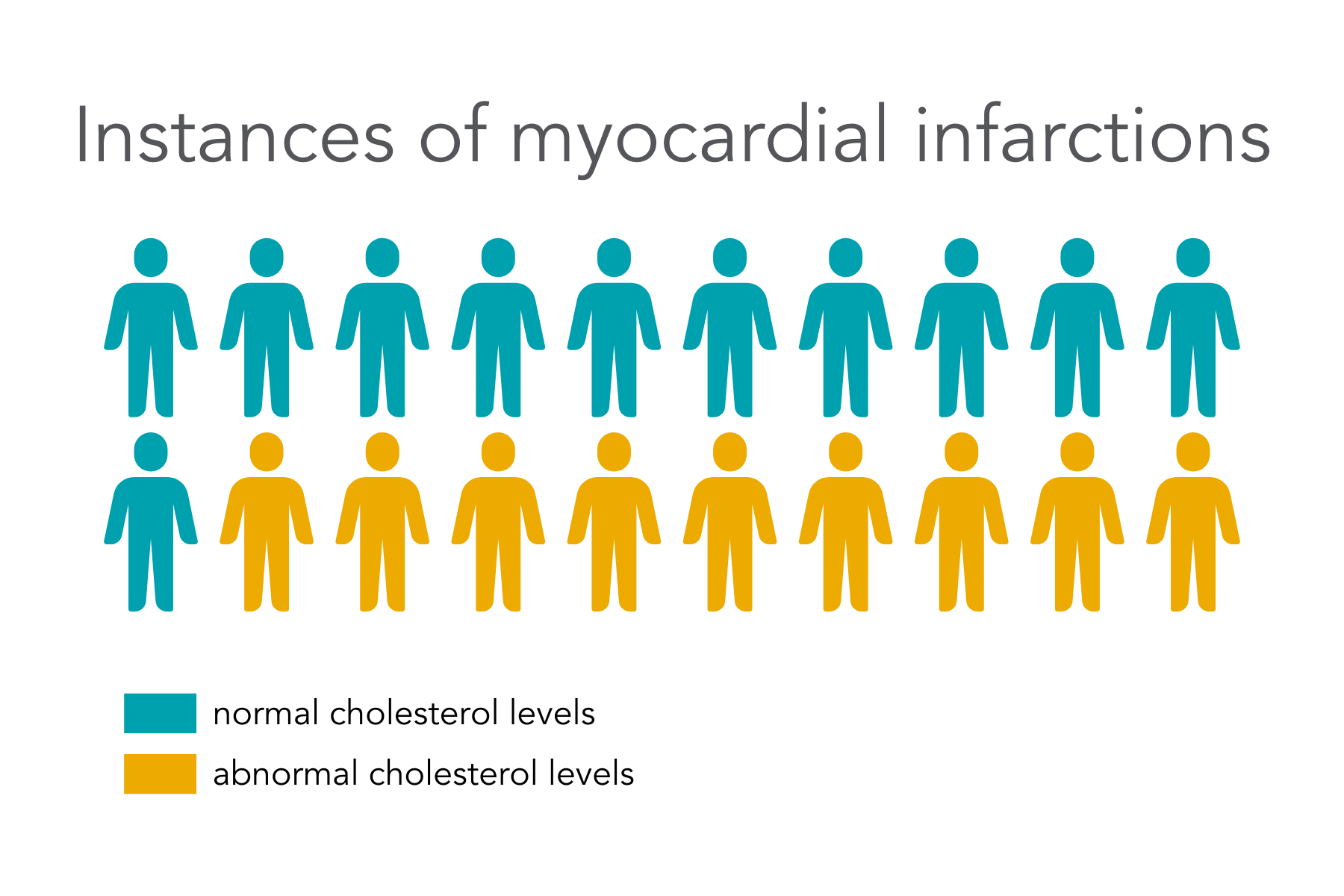
For the prevention-minded clinician, the question is: what intervention can mitigate the slight but real risk of an adverse event? The customary answer is to reduce the LDL-C levels. However, this may offer only a partial answer, because it neglects an important data point: that more than 50% of myocardial infarctions occur in individuals with normal cholesterol levels.2
A Novel Approach: Strengthen the Wall
A complementary perspective is available to practitioners: focus on the health of the arterial wall. This is because LDL is problematic only when it lodges in the subendothelial spaces and allows the accumulation of vulnerable plaque. Defending the endothelium against intrusion by excessive LDL clearly improves the risk profile.3
So what is the best way to protect the arterial wall? One answer is to restore and protect the endothelial glycocalyx (EGX), the micro-thin lining that governs the passage of cholesterol and other blood contents through the endothelium.
There are other benefits to focusing on the EGX, because this structure also regulates inflammatory responses throughout the entire vasculature. In addition, the EGX houses coagulation factors along with superoxide dismutase (or SOD, an important antioxidant), and it triggers the production of nitric oxide, which is key to blood pressure normalization.
Still curious?
Learn more about endothelial health with a 20-minute presentation by family practitioner Dr. Kristine Burke, detailing further the many roles of the endothelial glycocalyx, current research, and more.References
1. Khetarpal SA, Honigberg MC, Natarajan P. Implications of Premature Coronary Artery Calcification in Primary and Secondary Prevention of Atherosclerotic Cardiovascular Disease. JAMA Cardiology. Published online September 8, 2021. doi:10.1001/jamacardio.2021.3393
2. Miedema MD, Garberich RF, Schnaidt LJ, et al. Statin Eligibility and Outpatient Care Prior to ST‐Segment Elevation Myocardial Infarction. Journal of the American Heart Association. 6(4):e005333. doi:10.1161/JAHA.116.005333
3. Cahill PA, Redmond EM. Vascular endothelium – Gatekeeper of vessel health. Atherosclerosis. 2016;248:97-109. doi:10.1016/j.atherosclerosis.2016.03.007
IMPORTANT NOTICE:
The information on this webpage is for licensed healthcare practitioner education only, and is not to be disseminated to the general public.